I have had pt inujections epiduals surgery and nothing has helped. My doctor said there was nothing else they can do for me. I also have a stimulator in my back for cronic back pain. I feel I have no quality of life and all my friends have disappeard. I use a cane and a scooter, I can not stand for more than 10 minutes at a time.
been denied for disability and think about sucidie all the time. The ony thing stopping me is husband. I feel trapped and alone. QUOTE=GJZH;96790]I was wondering if anyone has Sacroiliac Joint Dysfunction and if you have it, did you have surgery for it? Has the surgery been successful? As I read more about this I think this might be a part of my pain and problems since my surgery. When I read this article it describes my pain, during the night especially. I really do not want more surgery. If you have had surgery, has it been successful for you? This seems like a very big surgery...I was wondering the success for it. Does anyone know?
A Patient's Guide to Sacroiliac Joint Dysfunction
http://www.eorthopod.com/eorthopodV2...f61e50b/area/5

Introduction
A painful sacroiliac joint is one of the more common causes of mechanical low back pain. Sacroiliac (SI) joint dysfunction is a term that is used to describe the condition - because it is still unclear why this joint becomes painful and leads to low back pain. Sacroiliac joint dysfunction can be a nuisance but it is seldom dangerous and rarely leads to the need for surgery. Most people who suffer from this problem can reduce the pain and manage the problem with simple methods.
This guide will help you understand
how the problem develops
how doctors diagnose the condition
what treatment options are available
Anatomy
What part of the back is involved?
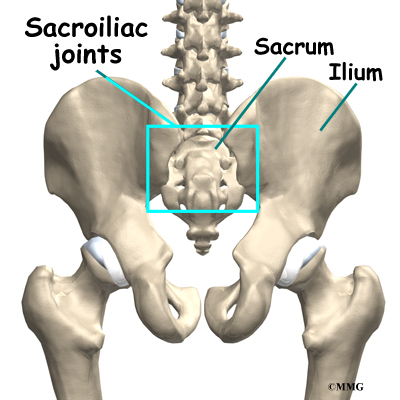
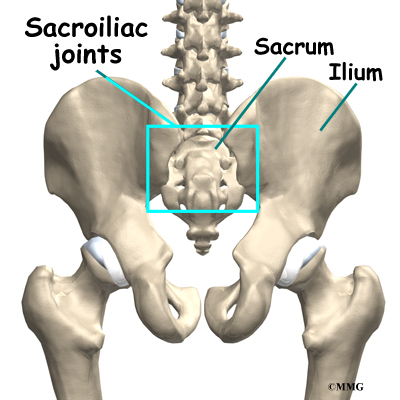
At the lower end of the spine, just below the lumbar spine lies the sacrum. The sacrum is a triangular shaped bone that is actually formed by the fusion of several vertebrae during development. The sacroiliac (SI) joint sits between the sacrum and the iliac bone (thus the name “sacroiliac” joint). You can see these joints from the outside as two small dimples on each side of the lower back at the belt line.
The SI joint is one of the larger joints in the body. The surface of the joint is wavy and fits together similar to the way Legos® fit together. Very little motion occurs in the SI joint. The motion that does occur is a combination of sliding, tilting and rotation. The most the joint moves in sliding is probably only a couple of millimeters, and may tilt and rotate two or three degrees.
The SI joint is held together by several large, very strong ligaments . The strongest ligaments are in the back of the joint outside of the pelvis. Because the pelvis is a ring, these ligaments work somewhat like the hoops that hold a barrel together. If these ligaments are torn, the pelvis can become unstable. This sometimes happens when a fracture of the pelvis occurs and the ligaments are damaged. Generally, these ligaments are so strong that they are not completely torn with the usual injury to the SI joint.
The SI joint hardly moves in adults. During the end of pregnancy as delivery nears, the hormones that are produced causes the joint to relax. This allows the pelvis to be more flexible so that birth can occur more easily. Multiple pregnancies seem to increase the amount of arthritis that forms in the joint later in life. Other than the role the joint plays in pregnancy, it does not appear that motion is important to the function of the joint. The older one gets, the more likely that the joint is completely ankylosed, a term that means the joint has become completely stiffened with no movement at all. It appears that the primary function of the joint is to be a shock absorber and to provide just enough motion and flexibility to lessen the stress on the pelvis and spine.
Causes
What causes this problem?
There are many different causes of SI joint pain. Pregnancy may be a factor in the the development of SI joint problems later in life. Also, if a person has one leg is shorter that the other, the abnormal alignment may end up causing SI joint pain and problems. Often, an exact cause leading to a painful SI joint condition can't be found. The joint simply gets painful, and the patient and provider don't have an answer as to why the joint has become painful.
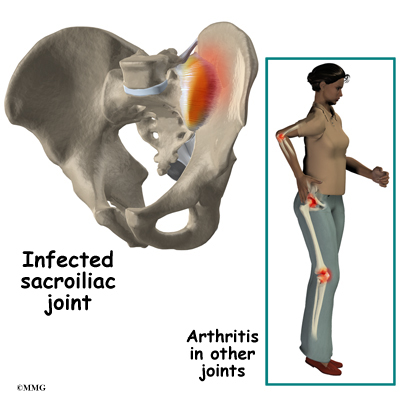
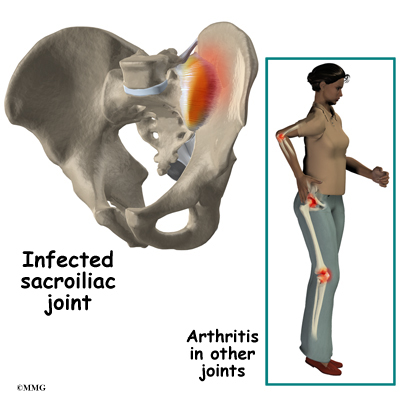
The SI joint is a synovial joint, similar to all joints such as the knee, hip and shoulder. Because of this, different types of arthritis that affect all the joints of the body will also affect the sacroiliac joint. This includes conditions such as rheumatoid arthritis, gout and psoriasis. The joint can be infected when bacteria that travel in the blood settle in the joint causing a condition called septic arthritis. This is perhaps the most worrisome cause of SI joint pain and may well require surgery to drain the infection.
Injury to the SI joint is thought to be a common cause of pain. Injury can occur during an automobile accident. One common pattern of injury occurs when the driver of a vehicle places one foot on the brake before a collision. The -->magnetic resonance imaging (MRI) scan can be used to look at the lumbar spine and pelvis in much more detail and to rule out other conditions in the area. The MRI scan uses magnetic waves rather than x-rays and shows a very detailed picture of the soft tissues of the body.
A computed tomography (CAT) scan may also be used to show a much more detailed look at the bone of the pelvis and the sacroiliac joint.
A bone scan is useful to see how the skeleton is reacting to any type of "stress," such as an injury, an infection, or inflammation from arthritis. This test involves injecting chemical "tracers" into your blood stream. The tracers then show up on special spine X-rays. The tracers collect in areas where the bone tissue is reacting strongly to some type of stress to the skeleton, such as arthritis and infection of the SI joint.
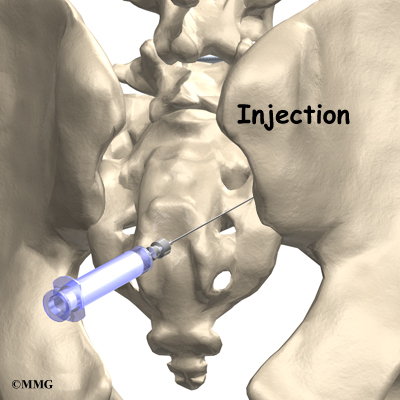
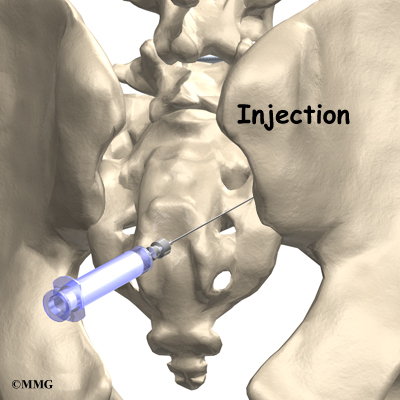
The most accurate way of determining whether the SI joint is causing pain is to perform a diagnostic injection of the joint. Because the joint is so deep, this must be done using X-ray guidance with a fluoroscope (a type of realtime X-ray) . Once the doctor places a needle in the joint, an anesthetic is injected into the joint to numb the joint. If your pain goes away while the anesthetic is in the joint, then your doctor can be reasonably sure that the pain you are experiencing is coming from the SI joint..
Treatment
What treatment options are available?
Nonsurgical Treatment
Doctors often begin by prescribing nonsurgical treatment for SI joint dysfunction. In some cases, doctors simply monitor the patient's condition to see if symptoms improve. Anti-inflammatory medications, such as ibuprofen and naproxen, are commonly used to treat the pain and inflammation in the joint. Acetominiphen (for example, Tylenol) can be used to treat the pain, but it will not control the inflammation.
Your doctor may ask that you rest your back by limiting your activities. The purpose of this is to help decrease inflammation and calm the muscle spasm. Some patients benefit from wearing a special brace called a sacroiliac belt. This belt wraps around the hips to hold the sacroiliac joint tightly together, which may ease your pain.

Patients often work with a physical therapist. After evaluating your condition, a therapist can assign positions and exercises to ease your symptoms. The therapist may design an exercise program to improve the strength and control of your back and abdominal muscles. Some therapists are trained in manipulative techniques that attempt to treat the pain in this manner. You may be able to learn how to adjust your SI joint yourself and ease the symptoms. If your physical therapist is not trained in manipulation, he/she may be able to suggest a chiropractic physician or osteopathic physician in your area who can provide this treatment.
If conservative treatment is unsuccessful, injections may be suggested by your doctor. As described above, injections are used primarily to confirm that the pain is coming from the SI joint. A series of cortisone injections may be recommended to try to reduce the inflammation in and around the SI joint. Cortisone is a powerful anti-inflammatory medication that is commonly used to control pain from arthritis and inflammation. Other medications have been injected into the joint as well. A chemical called hyaluronic acid has been used for years to treat osteoarthritis of the knee. This chemical is thought to reduce pain due to its lubricating qualities and the fact that it nourishes the articular cartilage in the synovial joints. The true mechanism of action remains unknown, but it has been used with some success in the SI joint. All of these injections are temporary and are expected to last several months at the most.
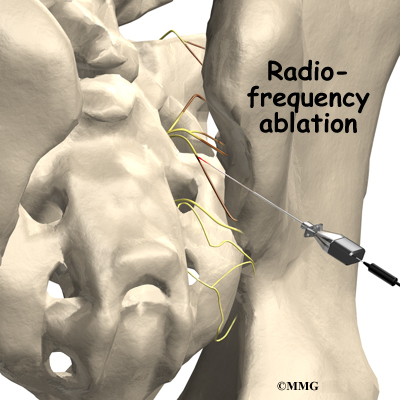
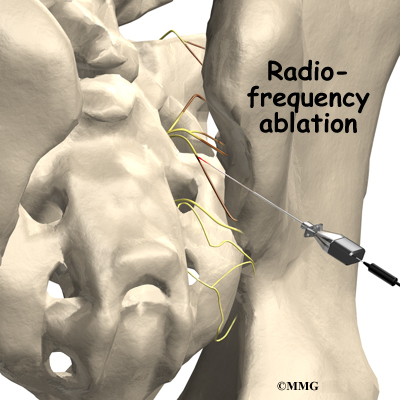
Another procedure that has been somewhat successful is called radiofrequency ablation. After a diagnostic injection has confirmed that the pain is coming from the SI joint, the small nerves that provide sensation to the joint can be "burned" with a special needle called a radiofrequency probe. In theory, this destroys any sensation coming from the joint, making the joint essentially numb. This procedure is not always successful. It is temporary but can last for up to two years. It can be repeated if needed.
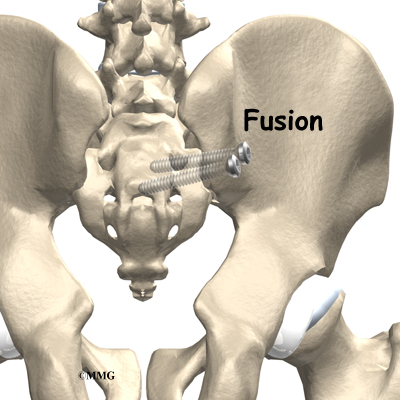
Surgery
Surgery may be considered if other treatments don't work. Surgery consists of fusing the painful SI joint. A fusion is an operation where the articular cartilage is removed from both ends of the bones forming the joint. The two bones are held together with plates and screws until the two bones grow together, or fuse, into one bone. This stops the motion between the two bones and theoretically eliminates the pain from the joint.
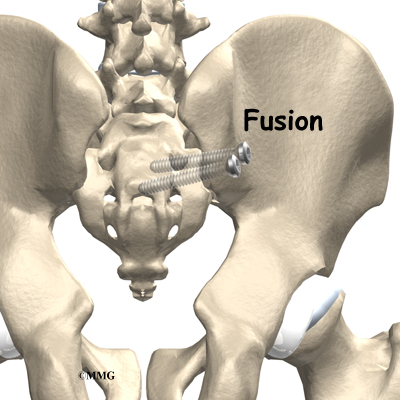
This is a big operation and is not always successful at relieving the pain. The operation is not commonly performed unless the pain is debilitating. SI joint pain is seldom this severe.
Rehabilitation
What should I expect as I recover?
Nonsurgical Rehabilitation
Doctors often recommend physical therapy for patients with SI joint dysfunction. Patients are normally seen a few times each week for four to six weeks. In severe and chronic cases, patients may need a few additional weeks of care.
When movement of a joint is limited, the pain and symptoms of SI joint dysfunction may worsen. Getting more motion can give you the relief you need for daily activities. If you don't have full range of motion, your therapist has several ways to help you get more movement including joint manipulation, stretching, and exercises. Active movement and stretching as part of a home program can also help restore movement and get you better faster.
Therapists commonly prescribe a set of stretches to improve flexibility in the muscles of the trunk, buttocks, and thighs. In addition to the treatment you receive by your therapist, you may be given ways to help your own SI joint if your pain returns. These exercises usually require that you position your hip and pelvis in a certain way and either stretch or contract and relax specific muscles. Follow the instructions of your therapist when doing these exercises.
If the SI joint has too much mobility and problems keep coming back, you may need extra help to stabilize the SI joint. You may be issued a SI belt to stabilize the joint. A belt like this can often ease pain enough to let you exercise comfortably.
You'll learn some exercises to help you build strength, muscle control, and endurance in the muscles that attach around the SI joint. Unfortunately, few muscles actually connect to both the sacrum and the pelvis. Key muscles to work are the gluteus maximus, as well as the abdominal and low back muscles.
After Surgery
You will normally need to wait at least six weeks before beginning a rehabilitation program after having SI joint fusion surgery. You should plan on attending therapy sessions for six to eight weeks. Expect full recovery to take up to six months.
During therapy after SI joint surgery, your therapist may use treatments such as heat or ice, electrical stimulation, massage, and ultrasound to help calm your pain and muscle spasm. Then you'll begin learning how to move safely with the least strain on the healing area.
As your rehabilitation program evolves, you'll begin doing more challenging exercises. The goal is to safely advance your strength and function.
As your therapy sessions come to an end, your therapist helps you get back to the activities you enjoy. Ideally, you'll be able to resume your normal activities. You may need guidance on which activities are safe or how to change the way you go about your activities.
When treatment is well under way, regular visits to your therapist's office will end. Your therapist will continue to be a resource. But you'll be in charge of doing your exercises as part of an ongoing home program.[/QUOTE]




 (if you're in america your lucky)
(if you're in america your lucky)


 Linear Mode
Linear Mode


